Introduction
My first encounter with Cancer was in 2004. I didn’t know then that it was a huge understated preview to the real show. This story is a personal account of my journey since the first appearance of liver cancer in 2019. I have learned many lessons along this path that have changed my viewpoint on life and have helped me succeed in this battle. The insights I have gained along this road may be of value to you, regardless of the difficulties you face. I present these insights in a separate article; reading both stories will give a view of the complete tapestry.
First Appearance
Discovering Cancer and Deciding on a Course of Action: June 2019
It all started on a Sunday morning early in June 2019. We were with our friends, having a great time picnicking and taking turns with my kayak on Emigrant Lake. It was only natural to feel some aches and pains, resulting from the intense physical activity. Yet, a dull pain in my upper abdomen felt somewhat different. It was still there the next day. Counter to my innate character, ignoring pains and aches unless severe, I saw my physician the next day. After a short physical exam, he sent me to have an ultrasound scan of my abdomen.
The following morning, I had the ultrasound scan done. Soon enough, the technician came out and asked me to stay for a CT. By noon, the results were in my physician’s hands, whom I saw right away. “Are you OK? Do you feel pain? Nausea?” were his welcoming concerns that really surprised me. “It seems that you have a rather large tumor in your liver”, he told us. “I am ordering a needle biopsy that an intervention radiologist will do. That is the only way we can really find out what it is.” We learned later that this profession is an MD that does certain minor surgical procedures guided by real-time x-ray imaging.
Friday we met with the radiologist. He told us that based on the tumor’s appearance in the CT scans, it is Intrahepatic Cholangiocarcinoma (ICC). He scheduled my biopsy to the following Monday. Back home, Connie started some research. She found that this procedure carries risks, pertinent to ICC, that were not worth taking. The first was reseeding. When the biopsy needle is pulled out of the tumor, some cancerous cells may be dispersed to other parts of the body. They then become a source for metastases; survival probability with metastases is extremely low. Furthermore, this procedure would void my eligibility to liver transplant, which could be one of the curative options. We called off the biopsy.
We weren’t in any mood to socialize at a dinner we were invited to with Rabbi David and some friends that night. We called Rabbi David to apologize for our absence. “Sure, not a problem, I understand,” he replied and added: “Dr. Dawn is one of our guests.” Dr. Dawn Lemanne is a well-known oncologist with an integrative approach that we already wanted to meet anyway. “OK!” I replied, “we’ll be there in 30 minutes with a large bowl of Israeli salad!” That is a great way to welcome Shabbat!
Dr. Dawn was very instrumental in laying out our way forward. She became the first member of my caring team. First, she pointed out the locations and experts that are best to deal with this type of cancer. She added rather unconventional instructions, such as, specific physical activities, special diet, sauna with cold showers and then some. Anything she suggested was backed up with scientific research and articles. backup. Sharing that information worked well with us, being scientists ourselves. Understanding the reasons and effects, backed up with statistics, motivated me to follow the suggestions. She ordered an MRI, more bloodwork, and a ctDNA – a liquid biopsy that looks for cancer traces in the blood.
It was time to hit the road to visit these experts, all over the West Coast. First was Dr. Anton Bilchik at Providence, Santa Monica CA. He explained his diagnosis and laid out his tentative approach to treat the illness. He asked for more tests before finalizing his recommendation: upper and lower GI endoscopy. He wanted to make sure that there was no other source hiding somewhere out there. We committed to provide him with the outcome of these tests and moved on to our next appointment. On our way to San Diego, we called a gastroenterologist, a member of our Temple, that we were already patients of. He scheduled the procedures to the first day after our return home.
Next was Dr. Brian Clary Head of Surgery at UCSD. Wow, was he prepared for our visit! He already had my case presented at their Tumor Board, and had the multidisciplinary team’s inputs. Yes, he also wanted to have the endoscopies done. However, not having the outcome of those didn’t hold him from sharing his thoughts with us, as his partners. He drew a decision tree and flow charts with all the what-ifs and the branches to track in each case. That was a language that both Connie and I, being engineers, could understand and relate to. At the bottom of his charts was the most likely outcome and a path forward that he recommended.
The tumor was rather big, about 5 inches, and occupied most of the larger right lobe of the liver. It came extremely close to the borderline of the smaller left lobe. The safest way was to take out the whole right lobe including the gallbladder. However, if he did it right away, the remnant left lobe would be inadequate to support me. His solution was Portal Vein Embolization (PVE). An intervention radiologist will block the incoming blood supply to the right lobe. During the following six weeks the left lobe will grow and will be sufficient to support life on its own. Then he can operate and take out the right lobe.
We drove back home, heading for yet another very busy week, starting with a PET Scan, Colonoscopy and Endoscopy.
It was the end of June when we traveled to OHSU in Portland to consult with Dr. Billingsley. After the initial pleasantries, he started explaining what are the possible reasons that caused the cancer. I said, stopping him on his tracks: “I’m not interested in it; tell me how you suggest we move forward.” He suggested to operate right away, setting a date to operate on the 9th of July.
We questioned him about the risks, and the issue of remnant liver we had learned from Dr. Clary. His answer was, “I should call Dr. Clary and tell him how to do that operation.” No humility at all. That was not the character of a doctor that we felt comfortable with. Yet, we feared that while waiting for Dr. Clary to operate the tumor would grow and possibly develop metastases. So, we signed the necessary paperwork to get the ball rolling with Dr. Billingsley .
Though, doubts continued to build up. Dr. Dawn’s experience with Dr. Billingsley aligned with our feelings from the meeting with him. Dr. Clary’s phone call to me on the 1st of July was the last convincing element. He emphasized the high risks involved in not letting the left lobe of the liver grow prior to the surgery. The next day we cancelled the scheduled surgery.
The Path towards Healing: July, August 2019 till March 2020.
It was clear: the risk in doing the surgery right away was too high to take. The ability to carve out the 5” tumor with negative margins all around was questionable. Furthermore, the remnant liver would not be sufficient to sustain me. The path Dr. Clary suggested seemed safer, even though a bit longer. Blocking the blood supply to the right lobe will also stop (at least temporarily) the growth of the tumor. The PVE was set for July 18th, and the surgery itself to August 26th. I told Dr. Clary about my commitment to lead the Hight Holidays services in Maui, HI, a month later. “I wouldn’t take that commitment to the bank” was his response!
The PVE was quite painful. The radiologist needed to have me conscious and able to follow instructions. Watching on the CT images what he had to accomplish, I felt awe for what he achieved. Due to some complications, the physician prescribed some antibiotics. Connie’s vigilance and advocacy brought the staff to change the prescription to another drug that wouldn’t harm the liver. Her vigilance and research abilities paid off, again.
Before leaving the Hospital Dr. Clary shared with us how he envisioned my next stay with them. There were some, not too high, risks that I wouldn’t make it out of the surgery. After the operation, I would stay for 2-3 days in ICU, and another 5-7 days in the medium care ward. On his way out, I asked him for a personal favor. He turned around, his entourage following him and inquired what was my request. I asked him to recite a prayer that Rambam used to recite before starting his work as a physician. I also asked to keep my media player and earbuds to play calming and spiritual music during the operation, He agreed to both.
Prior to the surgery, another CT. Lo and behold, The PVE did its job! The left lobe volume increased in 5 past weeks by more than 30%, and was large enough to support me.
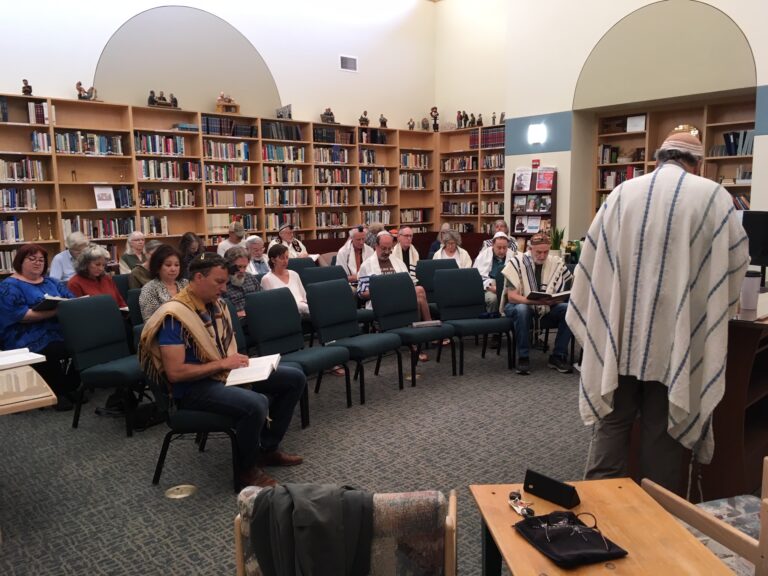
Monday morning, the day of the surgery, arrived. The playlist I made included songs of prayer, psalms and other sacred music that always moved me to tears. I knew that it would resonate and calm my soul even through the deep anesthesia. Before even entering the pre-operation room, I read a few psalms and recited ‘Sh’mah Yisrael’, holding both Connie and Aliza’s hands. I was truly at peace with any outcome of the surgery. It all will be OK, whatever it will be. I knew it. Back at home, folks held a healing morning service in which I participated via Zoom. Yet, another layer of reassurance.
Dr. Clary came in for a final check-in and encouragement. I gave him a copy of the Rambam’s Prayer for the Physician. He read it attentively and commented: “There is not a single word here that I disagree with. And I can use all the help I can get from any source.” I put the earbuds and turned on the music player, ready to be rolled into surgery.
The surgery took more than 6 hours. Dr. Clary emerged from the Operating Room, looking very exhausted according to Connie and Aliza. “The Rabbi is OK and the liver is in the pan” he told them. The first thing I noticed as I regained consciousness from the anesthesia was the song that played in my ears. It was the very same one that I remembered hearing before slipping into the induced coma. Another sign of Divine Intervention, or my imagination? I don’t know. Then, I took it as a sign from the Divine that everything is OK, as if the surgery didn’t happen.
A couple of hours later we all reconnected at the room where I was recovering. I was wired to monitors, had tubes delivering medications and liquids, while other discharged whatever needed to leave the body. Now, the task at hand was to recover, as quickly as possible. I had one proven remedy to do that: sleep, as much as I can. And that was what I did, or at least I tried to.
The heart rate monitor was a problem. Every now and then, perfectly aligned with my deepest sleep, it would start screaming. Nurses rushed in to “save my life”, but I was fine; just irritated by being awakened by the alarm. They then reset the threshold to a lower level. It didn’t take long for the alarm to go off again. Finally, the nurses set it to the lowest threshold available, 45 beats per minute. And still, it would go off a few times during the night. What a blessing! My heart is not going to be the one that kills me, the resident physician assured me.
The following morning, I already started walking, dragging all the machinery and plumbing with me. One by one the tubes were taken out, some were reinserted, and then taken out again. My walks included going up and down stairs; the physical therapist carried the pole with the whole enchilada alongside me. Friday, four days after the surgery, I was discharged. Considering that Dr. Clary expected me to stay in the hospital for at least eight days, my recovery was miraculous. After all, there was something I, and no one else, had to do: lead High Holidays services in Hawaii. We stayed nearby for three more weeks, to gain more strength and stamina until the final visit with Dr. Clary.

Walking around, one day after the surgery.
We were sitting in the examination room after the preliminary inquiries and vitals taken, waiting for Dr. Clary. Eventually, he came in, beaming with a grin. “Congratulations!” he greeted us. “What do we deserve this honor to?” was our response. He presented the pathological analysis of the right lobe that he took out. Indeed, it was Cholangiocarcinoma, and he succeeded in taking it all out, with negative margins. None of the cancer remained in, and there was no involvement of lymph nodes. It was stage 2 without metastases. Then he added the bottom line to his greetings: “you have 30% probability to live 5 years.” “Thank you, Dr. I WILL be in those 30%!” I promised him.

Coming back home after two months of absence was great, yet, it was not completely back to normal. We engaged in consultations with three professionals: the local practicing clinical oncologist, the UCSD gastrointestinal oncology specialist and Dr. Lemanne. What should we do next? Any adjuvant treatment? Or just surveillance? Dr. Lemanne was the only one who insisted that I do chemotherapy. We followed her recommendations which included a fast of 48 hours, starting 24 hours before the infusion. Research showed that the treatment is much more effective that way. I had 12 sets of infusion over a period of 5 months, without suffering essentially any side effects. The fast was the hardest part of the therapy. Then came COVID.
Second Appearance, March-April, 2021
Discovering a New Intruder, and Expelling It.
Following the completion of the Chemotherapy treatment, we started the quarterly surveillance protocol. It included an MRI of the abdomen, a CT of the chest and blood tests to check markers and ctDNA. And life was back to normal. Unfortunately, not for long. At the end-of-February scans, a small, ½” blip, has shown up in the liver, suspicious as a recurrence. A PET Scan confirmed that it was malignant. We engaged into high gear and mobilized the team to fight it once again.
Dr. Clary reviewed the images and set the date for a resection – cutting it out, with adequate margins. Dr. Lemanne recommended that, in addition to the traditional pathology and the tumor’s genetic analysis, we add another innovative test. The labs of Dr. Nagourney would take a sample of the live tumor, immediately after its excision. They would try a combination of chemotherapy drugs and evaluate which are the most effective in killing these cells. We mediated between all the interested parties in my tumor, and finally all got enough of it for their purposes.
Dr. Clary did the surgery on the 12th of April, and used the same incision he made for the previous one. Most of the time he spent on fighting the scar tissues that resulted from the former surgery. This one was child’s play, compared to the first operation. Two days later, on Wednesday, they kicked my butt out of the hospital (probably too much of a trouble maker). A week later we had the final post-operation visit with Dr. Clary. The pathology, again, showed that the margins were clear of any cancer cells. The recommendation was to continue with surveillance protocol only, without any adjuvant systemic treatment.
The Aftermath of the Event and its Impact on Me
This occurrence threw a wrench in my mind’s gearwheels. At best, the 5 year clock that Dr. Clary told us about, was now reset to zero. More realistically, it meant that another tumor was more likely to reappear than not. And probably, after the next one – should I survive it – will come another. And the time between recurrences may only be shorter. This realization did not decrease my resolve to continue doing everything to lessen the chances of a recurrence. Nor the determination to fiercely fight the next recurrence when it reappears. It did sharpen and focused my view on what was really important, and what I should focus on.
My need to visit Israel became urgent, ‘a must do right now’ feeling. We hadn’t been there since the spring of 2018. Initially because of cancer, and immediately following it were the travel restrictions imposed by the spread of Covid. Seeing my family and friends, spending time with the grandchildren and just breathing the air was rejuvenating.
I also started being more active in responding to my calling as a Rabbi. The experience I felt leading the High Holidays in Maui after the surgery was intense, in a very positive way. I knew that it was The Reason that helped me recover so quickly. The calling to serve my Jewish brethren was consuming. I felt that answering this calling will affect the souls of people for longer than I would live. It was a legacy I wanted to leave behind me. I also decided to start a website in which I will share my story and teachings that could inspire others.
I was – and still am – so fortunate to have Connie supporting me with these efforts. She did it full heartedly, regardless of her discomfort of the consequences of me becoming a congregational rabbi. Eventually, these efforts yielded fruits. We spent the High Holidays of 2021 leading a Conservative Congregation in Boca Raton FL. In January 2022 I became the rabbi of Temple Beth David in Spring Hill FL. This assignment really felt like the Voice of HaShem. My last name, Ben-David, means Son of David, David’s household; Beth David means the House of David. Spring Hill in Hebrew is Tel-Aviv, a city in Israel. I felt like I was going home.
Third Appearance, May-November, 2022
Finding the Recurrence and Returning Back Home
Shortly upon arriving to Spring Hill I met with the clinical oncologist at MOFFITT Cancer Center in Tampa. I showed him the results of my latest surveillance protocol that gave the “all clear” sign. We scheduled the regime of the next surveillance protocol and scheduled it to the first of May. The MRI revealed a new tumor in my liver. It was Monday; the oncologist had no suggestion yet, he needed to consult with his colleagues. We set another meeting for Thursday the same week to discuss my options. To my utter surprise, he cancelled the meeting. His assistant told me that instead I should contact and talk with an intervention radiologist. It certainly was not an attitude I liked.
I set the appointment with the assigned radiologist and prepared my questions. He offered a treatment called Yittrium-90 (Y90). We asked a lot of questions and pushed for other alternatives. During the conversation we learned that Dr. L, the clinical oncologist, referred my case to him, indicating the Y90 treatment. “Was there a Tumor Board that you participated in and considered other options?” we asked. The answer was negative. Yet another aspect neither of us liked, to say the least. We asked him to bring this case to a Tumor Board and consider other options, surgery included. A week later, Dr. L. shared their deliberation, essentially still offering the same Y90 treatment.
Back home, our team started reviewing the scans and considering options. We learned about the various ablation treatment options in addition to surgery. Our research indicated that the Y90 is mostly a palliative treatment rather than curative. Dr. Clary relayed to us the highlights of the UCSD Tumor Board. Essentially, surgery was not an option, because of the location of the tumor. It was too close to the heart, and in dangerous proximity to the colon. Instead, they recommended systemic chemotherapy that may make be a surgery possible after the treatment. Dr. Clary added that theY90 treatment will render any future surgery impossible. That in and of itself was enough to take MOFFITT’s physicians’ recommendation off the table.
It was obvious that it was time for me to pack and go back home. I talked with the leadership of Temple Beth David, and updated them with the news. We agreed that I would leave at the end of May, and continue supporting them remotely for another month.
Starting the Treatment That Led to Surgery
Together with Dr. Lemanne, we incessantly continued searching for a curative option. We searched for clinical trials that aimed to block the cell mutations which caused the cancer. We contacted several of them, just to be rejected for one reason or another. We visited MD Anderson in Huston TX and met with one of the lead researchers that ran a few clinical trials. After several tests, which included a tumor needle biopsy, he found that I did not meet his criteria of acceptance. We reached out to a leading GI oncology professional at Johns Hopkins, through our friend a math professor there. After she reviewed all the data, she offered an immuno-chemotherapy combination, that has just completed clinical trials.
It was now time to decide and act. We integrated the immune-chemotherapy that was just approved by the FDA with a tight scan schedule that Dr. Clary recommended. In that very meeting with Dr. Sander, my local oncologist, I asked her: “how long do I have?” “I am not ‘throwing in the towel” I added, “I am going to fight it as fiercely as I can. I just need to know so I can plan forward.” Her honest answer was: “you can plan for a year.” Right after the 4th of July, I started the treatments in the newly build Heimann Cancer Center.
The treatment regime was quite intense. A cycle started with a fast 24 hours prior to the infusion, that continued for a total of 48 hours. The infusion session itself was 6-7 hours long that included pre-medications, hydration, immunotherapy and two chemotherapy agents. A week later, another infusion session completed the cycle, with the 48-hours fast preceding it and two chemotherapy agents. This one was without the immunotherapy, and hence, an hour shorter. Then there was a break of two weeks till the next cycle would begin.
I entered the infusion hall for my first session early morning of July 7th. I was the first one to come in, and could pick any seat. What a view! I walked forward and took the very front seat so as to have nothing obstructing the sight. Later I noticed that the chair’s numerical designation was 18. What serendipity! The number 18, expressed by Hebrew letters (each letter in the alphabet has a numerical value) is Ḥay. The meaning of this word is ‘life’. Surely, Divine Providence guided me to pick up this chair, with a clear message: All will work out well. I requested this chair for all my future treatments.

Occupying Chair #18

The view from Chair # 18: the beauty of creation
After two of these cycles came the time to see what has happened inside my liver. The MRI scan showed a promising trend. The tumor that measured in June 3.5 by 2.7 by 2.8 cm shrunk to 2.7 by 2.5 by 2.3 cm. That is a significant reduction! We shared the images with Dr. Clary. He was happy with these findings. He suggested that I will take another MRI after completing two more cycles. If the tumor will not grow by then, he agreed that he can operate and excise it altogether. He wanted me to be off the therapy for six weeks prior to the surgery; that set the tentative date to the end of October.
I felt that I needed to travel to Israel after these two additional cycles. The timing was perfect: I could spend some of the High Holidays in Israel with my family and friends there. After all, it was already more than a year since I last visited the country. If all went well, it would be the perfect time to visit before the surgery. If the treatment did not perform as expected, it might be the only opportunity for me to go. The continued treatment with possible additional radiation therapy will take its toll and I wouldn’t have the strength to travel. I booked my flights and worked the details of the trip, as I continued occupying Chair #18.
A week before my departure, I had the MRI scan, after the completion of the additional two cycles. YES! The tumor continued shrinking and now was 1.9 by 1.6 cm! In terms of volume, it was now 20% of its original size. Dr. Clary confirmed that we are good to go with the operation, scheduled now to the 31st of October. That was my daughter’s birthday; yet another voice of the Divine Providence, saying that it is going to be OK.
The Surgery and its Outcomes
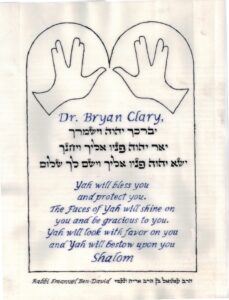
Monday the 31st arrived. Unlike the previous operations in which I was the first to go in, we had to wait. Finally, Dr. Clary came for the last check-in prior to the operation. I presented him a framed Priestly Blessing that I hand-written on parchment. At the back side of the frame was the Blessing of the Maimonides that he read before my first surgery. This gesture moved Dr. Clary, and for me it was as if he read the prayer again. It took him five hours to complete the surgery. Most of the time he fought through the many layers of scar tissues that resulted from the previous surgeries.
Recovery took four days due to a fever I had after the second day, yet, a record time for such a surgery. Dr. Clary said that to his surprise, he did not find any tumor in the liver. Not by palpation, nor by on-liver ultrasound scan. Nevertheless, he took out a wedge, based on landmarks he had from the previous scans. Then he took another wedge out, just to be on the safe side. His first concern was that he may have cut the wrong section. However, a ‘quick and dirty’ pathological analysis indicated that there weren’t any cancerous cells, but rather dead ones. With that, he assumed that the immune-chemotherapy and my own immune system completely killed the cancer.
It is time to go back home. Last visit with Dr. Clary and UCSD’s GI clinical oncologist to discuss the follow-up treatment. He recommended surveillance follow-up only; he claimed that my response to the treatment was off the charts. “Let’s keep this ammunition for future use, if and when the need will reappear” he said. We asked Dr. Clary, what if there will be another recurrence: will he operate on me? He, humble as always, said that he didn’t have experience with doing a third surgery on patients with cholangiocarcinoma. “Your body knows how to successfully fight it so hopefully you won’t have a recurrence” he said. “And if there will be one, we’ll deal with it then.”
Fourth Appearance, June, 2023
Discovery and Choosing the Treatment Option
Upon returning from our San Diego excursion, I did CT and MRI scans that would be the new baseline. The analysis of the scan was surprising. The radiologist reported that the previously measuring 1.9cm tumor was now 4.6cm! I dismissed it, attributing it to a mistake, or not considering the resection I underwent. And indeed, he amended the report after reading about my surgery. The next surveillance protocol came back with a clean bill of health.
Looking back at the timeline of the disease the pattern was clear. I had a recurrence about 11 months after completing the previous treatment. I finished chemotherapy after the first occurrence in May 2020, and discovered the next recurrence in February 2021. It took a year after that surgery in April 2021 to find another, rather large, one. My own immune system took care of it somewhere in October 2022. I was expecting something to show up in September, and wanted to take preemptive measures in June. I planned to discuss with my oncologists receiving a boost of immunotherapy during June Surveillance exams. I wanted to ready my body to fight the next one that could come anytime soon.
The MRI report of the June scan wasn’t yet ready when I met with my oncologist. We discussed the immunotherapy boost, and agreed that she will consult with the GI oncologist at UCSD about the details. We had a good visit, talking about books we read and what we glean from them. “I’ll call you when I will see the MRI report”, she promised. I left the office and headed to the parking lot, as my cellphone notified me of an incoming email. It was the MRI report. I glanced at it, and turned 180 degrees, reentering the clinic and requested to see Dr. Sander at once.
There was a small, ½ inch, new lesion, pretty much in the center of my liver. First order of business was to inform Dr. Clary about the news. I took upon myself to upload the MRI images to UCSD library, and Dr. Sander was going to send him a text message. Back at home I reviewed the MRI images. I found the little bastard nowhere near other organs. It seemed to me that instead of surgery it could be easily removed by ablation or some similar procedure. A few days later I had a PET Scan, that showed no other metastases. Good News! I was optimistic about our ability to handle it successfully.
Dr. Clary poured the loving yet ice-cold shower on us the following week. His initial evaluation of the images brought him to conclude that neither surgery or ablation were possible. The small tumor was too close to the main vein and bile ducts, rendering such procedures extremely risky. Instead, his initial thought was to do a combination of the previous immuno-chemotherapy with SBRT (Stereotactic Body Radiotherapy). We scheduled to meet Dr. Clary over Zoom to discuss the recommendations that his Tumor Board would make.
Meanwhile we started our research and study what is SBRT. Soon enough we found out that there is another form of SBRT that uses protons, rather than X-Ray photons. Proton Beam Therapy (PBT) can deliver much higher energy to the tumor than X-Ray radiation with much less collateral damage. Obviously, we preferred that treatment over SBRT. We contacted one of three facilities that are on the West Coast that offer this treatment in San Diego. We filled out forms and provided them with medical data even prior to our meeting with Dr. Clary. It was the last Thursday in June when we met him.
Dr. Clary explained again, using the MRI images why surgery and ablation were off the table. The Tumor Board recommended to start with the same immuno-chemotherapy I did before and reevaluate the progress before doing radiation. I pushed back and brought up the Proton Beam Therapy, telling Dr. Clary that we already contacted California Protons. Eventually, he agreed that it could be a good approach and took upon himself to call his colleague in California Protons in the next few days.
The very same day, we got a call from them, scheduling us to meet Dr. MacEwan over Zoom the next morning. We were in awe of Dr. Clary for is immediate action and the impact that his call had on Dr. MacEwan. Dr. MacEwan was well prepared for the consultation. He pulled on screen a comparison of the various PET Scans of my liver and pointed out the progress pattern. He assured us that he could kill this tumor altogether, without really risking the nearby vein and the bile ducts. They are much less sensitive to radiation and the beam is precisely shaped to hit the tumor only, he explained. We agreed to go forward with the treatment.
On the very same Friday I was summoned to report at California Protons on July 5th to start the treatment. We rushed to make all the arrangements for me to drive down to San Diego on the 4th of July. A day earlier I also received the first immunotherapy treatment. It so happens that the two augment each other and the result is better than doing each of them separately.
The Treatment and its Outcome

